courtesy
https://www.medicalnewstoday.com/articles/

Scientists have found ways to trigger the body's immune system to help fight cancer.
https://www.medicalnewstoday.com/articles/
Advances in cancer research
Every single year, thousands of cancer research projects release illuminating papers, and 2017 was no exception. And, as with previous years, there have been many fascinating breakthroughs in the quest to find new strategies to prevent and treat cancer.

Scientists have found ways to trigger the body's immune system to help fight cancer.
Around 1.6 million new cases of cancer are diagnosed in the U.S. each year, and nearly 600,000 people die from the disease.
Although chemotherapy, radiotherapy, and immunotherapy are typically used to fight cancer, these therapies do not work for everyone.
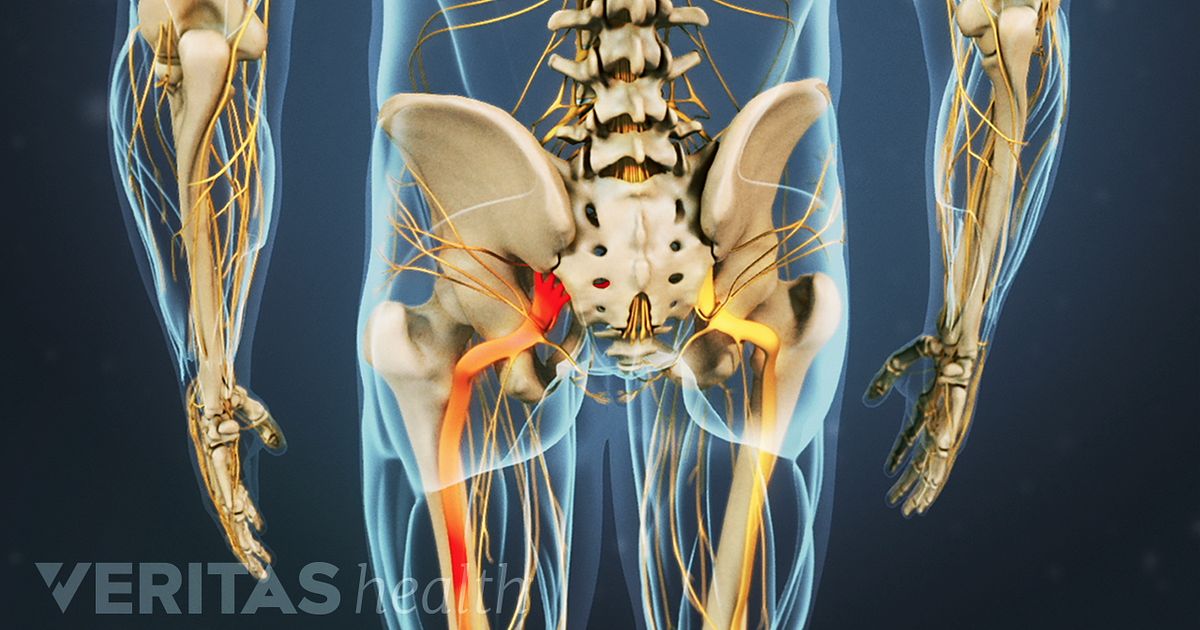
Scientists are continually studying the most effective ways to kill off cancer cells, and a handful of groundbreaking methods have entered the spotlight in the past 12 months. Two of these methods trigger a response from the body's immune system to fight off cancer.
The journal Science Translational Medicine published research demonstrating that poliovirus kills cancer cells and inhibits tumor regrowth.
Another cancer-killing technique heralded as more effective than convention cancer therapies is a process called caspase-independent cell death (CICD).
When cancer cells die from CICD, the immune system will swoop in to destroy any remaining ones that managed to evade CICD. When this method was tested in the laboratory on colorectal cancer tumors, almost all cancer cells were killed.
One surprising finding this year was the news that vitamin C is up to 10 times more effective than experimental drugs at preventing the formation of cancer stem cells.